COVID-19 coagulopathy is one of the most consequential effects of this disease. A recent study published in Science Translational Medicine indicates that circulating antiphospholipid autoantibodies may be, in part, responsible for the prothrombic effects of COVID-19.
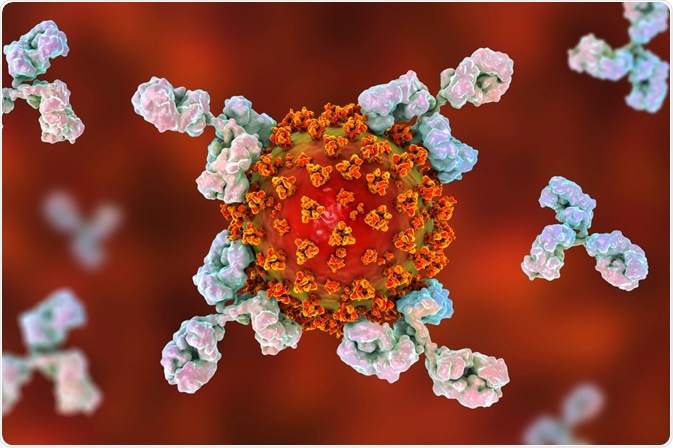 Image Credit: Kateryna Kon / Shutterstock.com
Image Credit: Kateryna Kon / Shutterstock.com
What are autoantibodies?
Autoantibodies, which are also referred to as natural antibodies, are antibodies that react with self-antigens. Under normal conditions, the human immune system is capable of discriminating between foreign substances, which are often referred to as non-self antigens, and antigens that are produced by the body’s own organs and tissues, which are also known as self-antigens.
However, individuals with autoimmune disorders like systemic lupus, thyroiditis, type 1 diabetes mellitus and primary biliary cirrhosis, for example, produce autoantibodies that target and react with their own cells, tissues and/or organs.
The interaction between these autoantibodies and self-antigens can result in inflammation, damage and/or dysfunction of various tissues and organs, depending upon the specific type of autoimmune disorder.
Immune mechanisms of COVID-19
As of December 9, 2020, a total of 1.56 million people around the world have died from COVID-19 as a result of infection by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Once the spike (S) protein of the SARS-CoV-2 binds to the ACE2 receptor present on the surface of the host cell, the virus can then enter the cell and begin to propagate and eventually move to the respiratory tract.
Whereas 80% of COVID-19 infected individuals will experience an infection that is predominantly restricted to the upper and conducting airways of the respiratory tract, it is estimated that the remaining 20% of patients will develop pulmonary infiltrates, some of which will experience very severe forms of the disease.
COVID-19 coagulopathy
While the majority of the people infected with COVID-19 typically experience mild to moderate symptoms, there are many people who experience a much more severe form of the disease.
Some of the severe complications of COVID-19 can include pneumonia, multi-system organ failure, acute respiratory distress syndrome, acute kidney injury, increased susceptibility to other viral and/or bacterial infections, as well as a unique form of coagulopathy that has been referred to as COVID-19 coagulopathy.
Early observations of COVID-19 coagulopathy characterized this disorder by mild thrombocytopenia, a small prolongation in prothrombin time, as well as elevated D-dimer in plasma. The presence of high D-dimer concentrations, which is a breakdown product of cross-linked fibrin, has been used to predict the patient’s risk of thrombosis, which correlates with disease severity, future ventilatory support requirements and an increased risk of mortality.
As compared to other types of intravascular coagulation disorders, the COVID-19 coagulopathy is unique in the fact that most patients will maintain normal concentrations of coagulation factors like factor VIII and von Willebrand factor, as well as fibrinogen and platelet levels.
Despite maintaining normal levels of these factors, COVID-19 coagulopathy is considered to be one of the most troubling complications of severe COVID-19, as it increases the risk of infected patients having both macrovascular and microvascular thromboses, either of which can increase the likelihood of the patient experiencing a stroke or myocardial infarction.
In fact, studies conducted in The Netherlands, France and Italy have found that 15% to 30% of critically ill COVID-19 patients experienced venous thromboembolism (VTE) and arterial thrombosis. In addition to these devastating clotting events, there have also been reports of that COVID-19 patients experience clotting of access catheters, dialysis membranes and extracorporeal circuits.
Some of the different mechanisms that have been proposed to be responsible for this abnormal clotting include a cytokine storm, hypoxic vaso-occlusion, as well as the virus directly activating both immune and vascular cells. Additionally, the presence of neutrophil extracellular traps (NETs) has also been reported in the blood of many severe COVID-19 patients, which can also contribute to prothrombic events.
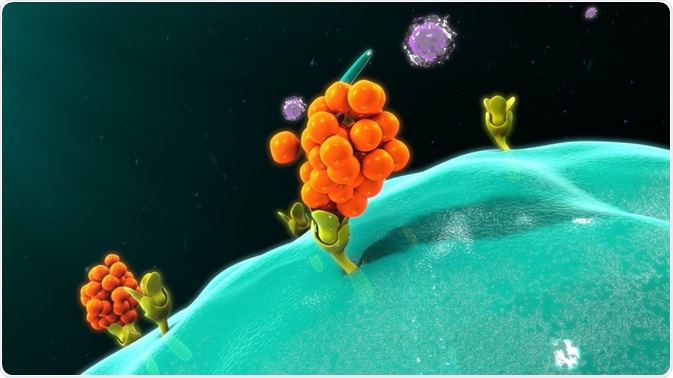 Image Credit: sciencepics / Shutterstock.com
Image Credit: sciencepics / Shutterstock.com
COVID-19 autoantibodies and coagulopathy
It is estimated that 0.5% of the population, or 1 in every 2000 individuals, suffers from an acquired autoimmune thrombophilia disorder known as antiphospholipid syndrome (APS). APS arises from the production of durable autoantibodies to phospholipids and phospholipid-binding proteins, which, taken together, are known as aPL antibodies.
These aPL antibodies interact with the surface of phospholipid-binding proteins such as prothrombin, b2 glycoprotein I (b2GPI), thrombomodulin, plasminogen, protein C and many others, which ultimately leads to the activation of endothelial cells, platelets and neutrophils.
The interaction between aPL antibodies and these cells causes the blood-endothelium interface to be at a greater risk of thrombosis. The diagnosis of APS typically occurs after a patient persistently tests positive for the presence of anticardiolipin autoantibodies (aCL antibodies) or anti-b2GPI autoantibodies (ab2GPI antibodies) in the blood.
A recent Science Translational Medicine study looked to determine whether the presence of aPL antibodies in COVID-19 patients could be related to COVID-19 coagulopathy.
In their work, serum samples obtained from 172 patients were evaluated for eight different aPL antibodies including aCL IgG, aCL IgM, aCL IgA, ab2GPI IgG, ab2GPI IgM, ab2GPI IgA, aPS/PT IgG and aPS/PT IgM.
Taken together, 89% of patients tested positive for at least one type of aPL antibody, the most prevalent of which included aPS/PT IgG, which was found in 24% of the patients. The researchers then sought to determine whether the presence of these aPL antibodies correlated with any clinical characteristics of COVID-19.
One of the most consistent findings was the activation of neutrophils, as indicated by calprotectin serum levels, and its associated presence with aPL antibodies. Activated neutrophils, in particular NET formation, have historically been associated with prothrombotic events that ultimately affect arterial, venous and microscopic vascular beds.
Conclusion
The discovery that severe COVID-19 patients are likely to produce aPL antibodies which, in turn, can potentiate the formation of NETs has several clinical implications. APS patients, for example, are often treated with heparin, corticosteroids and plasmapheresis.
Although both anticoagulation and corticosteroid treatments have proven useful in the treatment of COVID-19, plasmapheresis has not yet been fully explored and could thus offer a new method of effectively treating COVID-19 coagulopathy.
References
What are Autoantibodies [Online]. Available from: https://www.news-medical.net/health/What-are-Autoantibodies.aspx.
Chowdhury, M. A., Hossain, N., Kashem, M. A., et al. (2020). Immune response in COVID-19: A review. Journal of Infection and Public Health 13(11); 1619-1629. doi:10.1016/j.jiph.2020.07.001.
Coronavirus disease 2019 (COVID-19) [Online]. Available from: https://www.mayoclinic.org/diseases-conditions/coronavirus/symptoms-causes/syc-20479963.
Chan, N. C., & Weitz, J. I. (2020). COVID-19 coagulopathy, thrombosis and bleeding. Blood 136(14); 381-383. doi:10.1182/blood.2020007335.
Zuo, Y., Estes, S. K., Ali, R. A., et al. (2020). Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Science Translational Medicine 12(570). doi:10.1126/scitranslmed.abd3876.
Lerma, L. A., Chaudhary, A., Bryan, A., et al. (2020). Prevalence of autoantibody responses in acute coronavirus disease 2019 (COVID-19). Journal of Translational Autoimmunity 3. doi:10.1016/j.jtauto.2020.100073.
Further Reading