Peripheral arterial disease/peripheral artery disease (PAD), or peripheral vascular disease (PVD) is a common condition where bodily arteries become narrowed due to a build-up of fatty plaques (atherosclerosis).
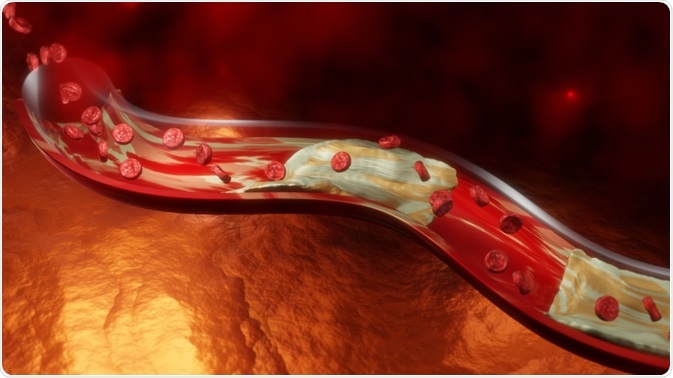 Image Credit: Anshuman Rath/Shutterstock.com
Image Credit: Anshuman Rath/Shutterstock.com
What causes peripheral arterial disease?
Atherosclerosis is the build-up of fatty deposits called atheromatous plaques within the walls of major blood vessels (arteries) causing a gradual narrowing of their lumen diameters to restrict blood flow and oxygen transport to tissue over time. PAD is essentially caused by atherosclerosis of peripheral arteries (especially at major branch points).
Atherosclerosis in the heart is referred to as coronary artery disease and if it occurs in the brain it is called cerebrovascular disease, including stroke and vascular dementia. PAD refers to atherosclerosis of other parts of the body, such as in the feet and legs. PAD is estimated to affect over 200 million people worldwide and its prevalence increases with advancing age.
What are the symptoms of peripheral arterial disease?
The majority of people with PAD; especially in earlier stages, will not have any noticeable symptoms. Once the affected areas e.g., legs, progressively worsen, symptoms will become more apparent.
The most common symptom of PAD that appears first is known as intermittent claudication – which is muscle pain or cramping upon physical exertion that is relieved upon rest. In addition, the particular region suffering from PAD may also have a lower temperature compared to the rest of the body as well as some redness.
Other symptoms that may develop can include:
- Lack of growth of nails or hair in the affected region
- Pale or discolored skin
- Limb weakness and/or numbness
- Pins and needles/tingling sensations
- Sores that do not heal quickly may also become infected
If left untreated, PAD can progressively worsen leading to critical limb ischemia (sudden drop in flow to the affected region) and gangrene (death or necrosis of tissue within that region). This could be limited to extremities such as toes, or larger areas of the leg, for example. Unfortunately, tissue necrosis caused by critical limb ischemia is irreversible and may require amputation.
What are the risk factors for peripheral arterial disease?
- Smoking – the biggest risk factor for PAD is smoking, where smokers have on average a 10x fold increase in risk of developing PAD.
- Diabetes – diabetic patients have on average a 2-4x fold increase in risk of developing PAD.
- High blood pressure – hypertension increases the risk of developing PAD by 2.5-4%
- High blood cholesterol – dyslipidemia/hyperlipidemia increases the risk of atherosclerosis – the primary cause of PAD
- Sedentary lifestyle – lack of physical activity or exercise
Other risk groups that have been identified who may have an increased risk are:
- Family history of PAD or heart/cardiovascular diseases
- Certain ethnicities/ethnic origins e.g., African American individuals
Peripheral artery disease: Pathophysiology, Causes, Symptoms, Diagnosis and Treatments, Animation
How is peripheral arterial disease diagnosed and treated?
PAD is diagnosed by performing a physical examination and confirmatory testing by a physician. Specific examinations are made to assess PAD which include:
- Ankle-brachial index (ABI) test – used to compare the blood pressure in the affected region (e.g., leg) compared to a non-affected region such as the arm.
- Checking for weaker pulses in the affected area
- Listening to poor blood flow in the affected area
- Assessing the color of the affected region, as well as examining any sores and swelling
- Blood tests to assess blood cholesterol, fat and sugar levels
Treating PAD before it progresses is important in minimizing the complications and potentially devastating consequences that can arise. These include modifying risk factors, lifestyle and treatments for atherosclerosis, diabetes, hypertension & dyslipidemia, etc.
The most common ways to minimize the risk of PAD worsening is to:
- Stopping smoking
- Increased levels of physical activity and exercise (30-45 minutes 3 or 4 times a week for at least 12 weeks) can substantially improve claudication
- Improving diet to reduce saturated fat/high cholesterol food intake (to combat hypercholesterolemia/obesity) as well as reducing high-salt and high-sugar foods in combatting hypertension and diabetes
- Managing hypercholesterolemia by taking statins to reduce cholesterol levels and antiplatelet drugs (such as daily aspirin) to reduce blood clot formation
Surgical interventions can include:
- Angioplasty – a surgery performed to open up narrow or blocked arteries by inserting an inflatable balloon to flatten the plaque. This is usually followed by inserting a stent to minimize arterial narrowing in the future.
- Bypass surgery – another functional blood vessel, or artificial vessel is surgically placed to divert blood flow from the blocked artery to form a ‘bypass’ way around the blockage.
In summary, peripheral arterial disease (PAD) is the atherosclerosis (build-up of fatty plaques and narrowing of arteries) of peripheral arteries e.g., in the leg. Symptoms usually present later in disease, often characterized by intermittent claudication – pain upon physical exertion, in addition to the affected area feeling colder and having a lower pulse/blood pressure. PAD can be treated before tissue death (necrosis) occurs by a variety of physical, pharmacological and surgical interventions, however, if left untreated can result in gangrene and in need of amputation.
References
Further Reading