COVID-19 is a respiratory disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Whilst the majority of COVID-19 cases are mild or moderate, a small proportion are severe and can lead to difficulties with breathing and pneumonia. Understanding what SARS-CoV-2 does to lung cells will enable better treatments for severe COVID-19.
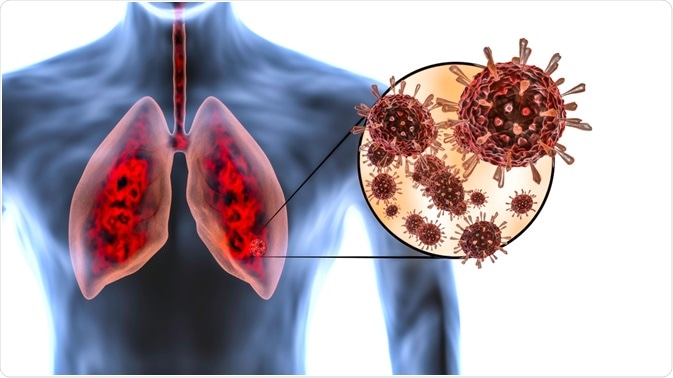 Image Credit: MarcinWojc / Shutterstock.com
Image Credit: MarcinWojc / Shutterstock.com
Asymptomatic COVID-19
A large proportion of healthy individuals (as many as around 40% or more) who test positive for COVID-19 do not exhibit any noticeable symptoms, however, are still able to transmit the disease. It is thought that the vast majority of asymptomatic patients are younger. Whilst asymptomatic individuals who test positive for COVID-19 may not overtly show any signs of lung damage, new evidence suggests that there may be some subtle changes that occur in such patients, potentially predisposing asymptomatic patients for future health issues and complications in later life.
Case studies from recovered asymptomatic COVID-19 patients have shown lung abnormalities using CT scans. For example, take the case of the Diamond Princess cruise ship, where there was an infamous outbreak of COVID-19 at the beginning of the pandemic in February 2020.
73% of positive COVID-19 cases on board the Diamond Princess cruise ship were asymptomatic, of which 54% showed lung opacities (ground-glass opacities; GGO) which reflects the filling of the air spaces in the lungs with fluid relating to edema, fibrosis (scarring) and inflammation in the lungs.
However, it is important to note that whilst a majority of patients on board the Diamond Princess cruise ship were asymptomatic, the overall age of the group was older, thus there may be age-dependent effects that occur, which may not occur to such an extent in younger individuals.
Symptomatic COVID-19
In most people, COVID-19 leads to very mild (barely noticeable), mild (weak) or moderate (more pronounced, but manageable) symptoms, though a significant proportion do not exhibit any symptoms at all (asymptomatic; see above). The variances in clinical presentation may be attributed to high viral load, age, pre-existing health conditions, ethnicity/demographics amongst other lifestyle, genetic and environmental factors.
As with variances in clinical presentation, there is a huge variance in the pathological features associated with COVID-19 from asymptomatic individuals through to those with the most severe disease. Unfortunately, a majority of pathological and imaging data come from those hospitalized with COVID-19 rather than non-severe symptomatic patients who do not routinely visit the hospital to receive diagnostic check-ups. As such, the effects of COVID-19 on the lungs are largely investigated in severe disease only, with a few case study exceptions.
Post-mortem lung samples from patients who died from COVID-19 (who had severe disease; acute respiratory distress syndrome (ARDS)/pneumonia in requirement of intensive care unit admission) in Italy displayed extensive alveolar damage, capillary congestion, necrosis of pneumocytes (cells that line lung air spaces forming the barrier of gas exchange in lungs as well as producing surfactant which reduces surface tension in the lungs) and interstitial and alveolar edema (fluid in air spaces).
Furthermore, there was evidence of type-2 pneumocyte hyperplasia (increased number of surfactant secreting cells), squamous metaplasia with atypia (non-cancerous changes to lung epithelia) and platelet-fibrin thrombi (blood clots) in small arterial vessels, with increases in D-dimer levels in the blood. All of these changes severely impact the ability of lungs to function (breathe) and oxygen to be absorbed into the bloodstream leading to severely depleted blood oxygenation levels (hypoxia) which then require patients needing ventilators. The higher the level of pathology, the higher the risk of death from COVID-19.
Those that suffer from more severe COVID-19 with extensive lung damage go on to develop pulmonary fibrosis – which is the unsuccessful reconstruction of damaged alveolar epithelium and the presence of fibroblasts and the excessive deposition of hyaline and collagen (among other extracellular matrix proteins) which remodel the lungs.
This can progress with the compression of lung tissue, damaging pulmonary capillaries and leading to death by respiratory failure. Specific treatments targeting inflammation, oxidative stress and specific cytokines (such as anti-inflammatories, steroids, fibrinolytic agents or specific antibodies) may be useful in preventing pulmonary fibrosis from progressing, especially if used early on.
A case-study of a 31-year-old woman who died from COVID-19 revealed extensive lung damage. 7 days prior to her death, she complained of persistent cough and remained confined to her home after seeking medical advice. Whilst the woman was young, she was morbidly obese (BMI 61.2kg/m2). The autopsy revealed heavy lungs which were firm and rubbery with hemorrhagic edema bilaterally, pleural effusion (build-up of fluid) as well as signs of extensive shock characterized by variegated appearance of the liver and kidneys.
Histopathologically, her lungs revealed alveolar damage (as described previously) with the deposition of fibrin-thrombi (clots) within alveoli. Furthermore, extensive immune system cell infiltration into the lungs was present including T-lymphocytes and megakaryocytes. Thus, this shows the extent of damage that can occur to lungs from COVID-19 if left untreated, especially in those that are clinically vulnerable (e.g., obesity and heart diseases). Thankfully, the majority of deaths do not occur at this age range, and with increased knowledge of better treatments, many of these pathologies can be mitigated and perhaps even reversed in some patients.
How COVID-19 Affects Your Lungs
Long-term lung damage
As COVID-19 is a relatively new disease, the full long-term effects of COVID-19 are still poorly understood, and new developments continue to arise with respect to observational case and cohort studies (including follow-up check-ups by doctors). However, based on initial case studies from those with moderate-severe disease (such as those that develop pneumonia), the initial damage to the lungs can persist leading to decreased lung function which may impact on activities of daily living i.e., quickly getting out of breath when climbing some stairs. Pulmonary fibrosis is one of the major complications of severe COVID-19.
Even with fully recovered symptomatic patients, there may be some long-term lingering effects that persist for several months. Up to 23% of recovered SARS patients (similar to COVID-19) displayed reduced lung exercise capacity and pulmonary function a year after infection. Thus, it would be safe to assume a similar level of long-term reduction in lung function with respect to COVID-19; especially in those with moderate/severe symptoms.
In summary, COVID-19 is primarily a respiratory disease that leads to flu-like symptoms with additional specific neurological symptoms. Depending on the severity of the disease, extensive and long-lasting damage to the lungs can occur, which may persist well after the infection. More research is needed to determine the full extent of damage to the lungs in a variety of patients across different age groups and severities, as well as assessing long-term effects to the lungs.
References
Further Reading