The position of the baby inside the uterus keeps changing during pregnancy. At the time of delivery, the best position for the baby to be in is the head-down position. This position allows safer and easier passage of the baby via the birth canal and minimizes complications during child birth. However, this is not always the case and other fetal positions are common.
What is breech?
A fetus is said to be in a breech position if the baby is in a bottom-down position instead of head down. In breech presentation, the buttocks or foot / feet of the baby presents at the bottom of the uterus instead of the baby’s head.
During the last few weeks of pregnancy, health care providers check the position of the fetus with the help of a clinical examination and an ultrasound. In case breech presentation is confirmed, doctors discuss the matter with the woman and her partner and decide on options that will ensure a safe delivery.
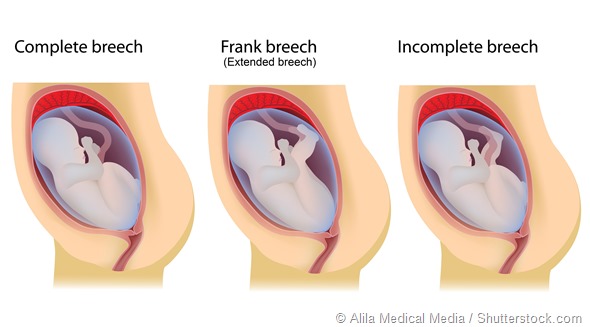
Types of breech
Depending on which part is presenting as the lowest part of the fetus during a clinical examination, breech is classified into 3 types.
Extended breech – In this position, the hips of the baby are flexed and its legs are extended at the knee joint. The baby appears bottom first with its feet seen near its head.
Complete or flexed breech – Here, both the hips and knees of the fetus are flexed, the feet are stretched up and not seen below the level of the buttocks.
Footling breech – In this type of breech, one or both feet of the fetus extends downwards and lowers over the cervix, presenting as the lowest part of the fetus.
Risk factors contributing to breech presentation
Some risk factors at the maternal and fetal level can increase the chances of breech presentation. They are as follows:
Maternal factors
- Previous breech birth
- First pregnancy
- Early labor
- Abnormal shape of the uterus
- Presence of fibroids in the uterus
- Excess or low levels of or amniotic fluid
- More than one baby in the womb
- Placental abnormalities such as placenta previa in which placenta is on the lower part of the uterine wall and blocks the cervix
Fetal factors
- Short umbilical cord
- Extended fetal legs
- Abnormal fetus
- Poor growth of the fetus
Clinical examination
In late pregnancy, a clinical examination is carried out to assess the presentation of the fetus.
Breech presentation is suspected in the following cases:
- During abdominal examination, the lowest part of the fetus or the presenting part feels irregular and a hard round part is found in the fundus, which is the upper part of the uterus.
- Heart sound of the fetus comes from the upper portion of the abdomen, typically above the navel or the umbilicus.
- During pelvic examination, the hard round head cannot be felt in the pelvis and instead the soft buttocks and / or the feet of the fetus are felt. Once the membrane breaks, thick, dark green feces called meconium may be present
When a breech presentation is suspected by 37 weeks of pregnancy, an ultrasound may be done to confirm the type of breech - extended, flexed, or footling breech - and exclude fetal head hyperextension and placenta previa.
In case of fetal head hyperextension beyond 90 degrees, there is a high risk of damage to the spinal cord during vaginal delivery and hence delivery via caesarean is recommended. The chance of a breech baby spontaneously turning into a cephalic position declines as pregnancy advances, but it is still possible in nearly 25% of women after 36 weeks.
References
- https://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000623.htm
- https://thewomens.r.worldssl.net/
- http://apps.who.int/iris/bitstream/10665/43972/1/9241545879_eng.pdf
Further Reading