Atypical moles, otherwise known as dysplastic nevi, are known to increase the risk of certain types of skin cancer, namely, melanomas. These cancers are becoming more common all over the world, and currently make up 4 percent of skin cancers. They are responsible for the death of 8 out of 10 people with a cutaneous malignancy.
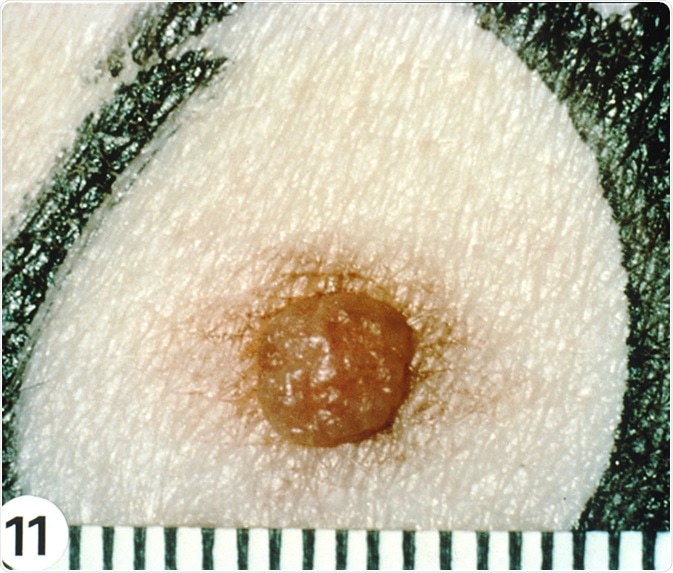
Dysplastic Nevi - The delicate, hazy, tan macular rim of this lesion, although not clinically dramatic, represents persistent melanocytic proliferation beyond the lateral limits of the common mole at its center. Image Credit: National Cancer Institute
Early detection of melanoma is essential to help achieve a remission, for which reason the risk factors need to be identified and surveillance instituted when these factors are present. The 5-year survival rate is around 95 percent in stage 1 melanomas, but only about 15 percent in stage 4.
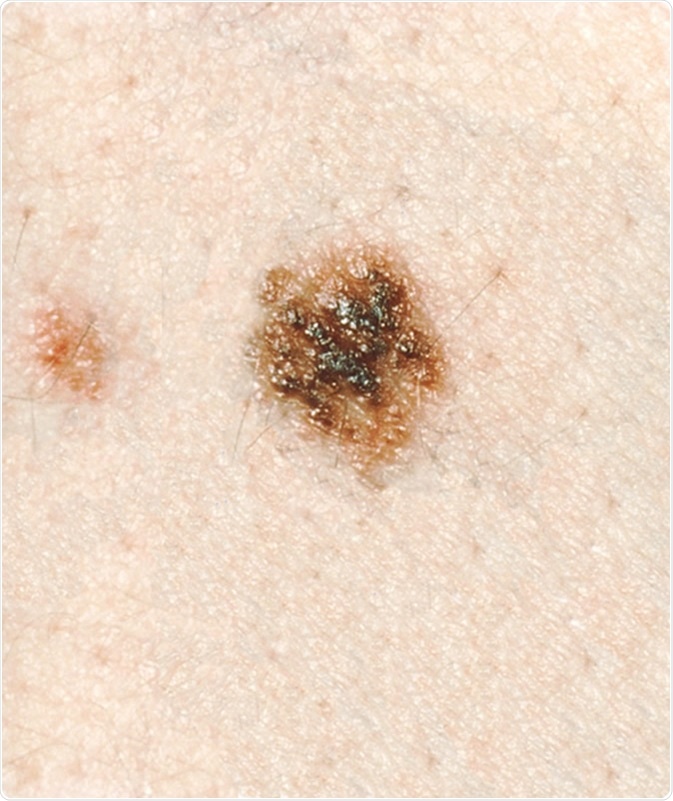
Dysplastic Nevi - This lesion has a dark brown, "pebbly" elevated surface against a lighter tan, macular background. The irregular, indistinct margin of the nevus helps to distinguish it from the small congenital-pattern nevus, which some dysplastic nevi closely resemble clinically. Its distinctive morphology, not its size (6 by 6 mm), identifies it as a dysplastic nevus. Image Credit: visualsonline.cancer.gov
Atypical Moles and Melanoma Risk
Both genetic and environmental factors play a role in the genesis of melanoma, and among these is the presence of multiple dysplastic nevi, common nevi, and familial atypical multiple moles and melanoma (FAMMM) syndrome as well as the atypical mole syndrome (AMS). The dysplastic nevus was first considered a precursor to sporadic melanoma.
The risk of melanoma is increased by at least ten times in individuals with five or more dysplastic nevi, while it is 12 times the population risk in those who have ten or more of these lesions. Dysplastic nevi show disordered structure and cellular atypia, but not malignant changes, even in situ. About 20 percent of dysplastic nevi do undergo malignant transformation, but the others remain stable throughout life or even regress. From this perspective, a dysplastic nevus may be thought of as a potential and non-obligate precursor of melanoma.
The risk of melanoma occurring in any given dysplastic nevus has been calculated to be approximately 1 in 30,000 for men and 1 in 40,000 for women, which confirms that their primary importance is a risk marker rather than a precancerous condition in itself. The risk for melanoma with increased numbers of dysplastic nevi ranged from approximately 5 to 12, and constituted an independent risk factor for melanoma. This risk also correlated with a higher number of small and large nevi.
Surveillance of Dysplastic Nevi
Individuals with increased risk for melanoma development are identified partly on the basis of a high number of dysplastic nevi as well as common nevi. Other genetic, host, and environmental factors also operate to produce this tumor.
Surveillance begins with regular check-ups of the whole skin by a physician, which includes photography of the whole skin if any dysplastic nevi are found. How often such visits are conducted depends upon the age, gender, and type as well as level of activity of the lesions. Any lesion which shows changes that raise the question of malignancy requires excision biopsy. In families with a history of melanoma, these measures help reduce the emergence of new melanomas, and in the early detection of these tumors.
Protection of the skin against solar damage, by sunburn and suntan either by natural sunlight, tanning beds, or the use of sunlamps, is necessary, especially if a positive family history is given.
Regular evaluation of the skin should be taught and recommended to the patient as well. The use of photographs of nevi identified earlier will help detect changes earlier. Most changes are innocent, but if any suspicious alterations are present, excision biopsy is mandatory, usually with a 2mm margin. Dermoscopy is also helpful in identifying which lesions need to be excised for biopsy when performed by a skilled examiner.
Monitoring of individuals from families with AMS should begin around puberty, when the risk for melanoma starts to increase. Self-assessment of the skin should be taught as a less expensive method of monitoring, while ophthalmoscopic assessment should be considered on an annual basis, at least, to detect uveal melanomas.
Prophylactic Removal of Dysplastic Nevi
Prophylactic excision of all nevi is not required or recommended for several reasons. First, very few dysplastic nevi actually go on to turn into melanomas, which makes the removal of all nevi unnecessary. Moreover, it is impossible to predict exactly which nevi will progress, apart from the fact that melanomas very often always arise de novo rather than from nevi. This would make follow-up still as frequent and mandatory as before in nevus-prone individuals, since the risk remained as high as before. In fact, the removal of all dysplastic nevi might harm the individual by promoting a false sense that their risk has now gone down, making them less careful to come in for regular screening.
References
Further Reading