Unregulated autophagy results in the inefficient sequestration and clearing of damaged cellular components that are essential for cell survival and function. This can cause a number of diseases. It is therefore crucial to understand the regulatory processes that govern autophagy.
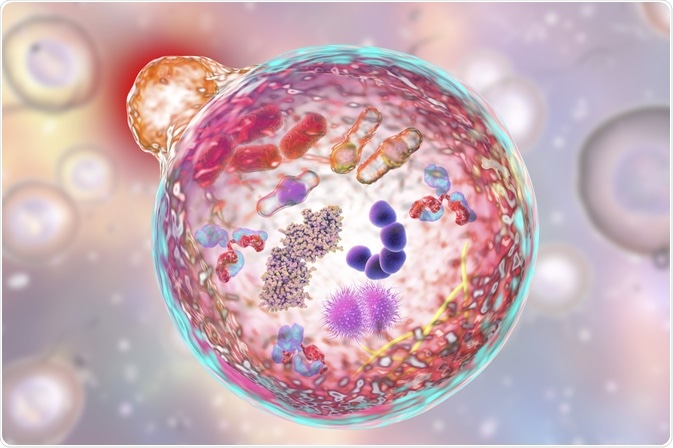 Kateryna Kon | Shutterstock
Kateryna Kon | Shutterstock
Autophagy is an evolutionarily conserved self-degradation process of cellular components. It plays a role in development, aging, infection, immunity and several human diseases. Mammalian autophagy refers to three cellular processes:
- Macroautophagy involves the formation of autophagosome to engulf the cellular components.
- Microautophagy involves direct uptake of the cellular components by the lysosomal membrane.
- Chaperone-mediated autophagy is a selective form of autophagy that is observed only in mammalian cells. It involves the recognition of the KFERQ-related motif on the substrate by Hsc70. This allows the substrate to be delivered to the lysosome.
What is macroautophagy?
Macroautophagy is a multi-step process that proceeds in distinct stages, and different types of ATG proteins are involved in these steps that form the core autophagic machinery.
Initiation
Macroautophagy starts by budding of a membrane off of the endoplasmic reticulum to form a pre-autophagosome. This developing cup-shaped membrane requires a protein complex consisting of Unc-51-like kinase 1 (ULK-1), ATG13, ATG101, and FIP200.
Nucleation
As the double-membraned pre-autophagosome elongates, it requires a protein complex comprising of vacuolar protein sorting 34 (Vps34), Vps15 and Beclin 1. ULK1 activates Beclin1 through phosphorylation.
The Beclin1-Vps34-Vps15 complex is a class 3 phosphatidylinositol 3-kinase (PI3K) that produces (phosphatidylinositol 3-phosphate (PIP3) from phosphatidylinositol 2-phosphate (PIP2). The increase in PIP3 leads to the recruitment of WD-repeat protein interacting with phosphoinositides (WIPI) proteins to the pre-autophagosomal membrane.
Elongation
As the pre-autophagosome elongates and matures, microtubule-associated protein 1 light chain 3 (LC3-1) is recruited. This, along with the ATG5-ATG16-ATG12 complex targets specific substrates to the developing autophagosome.
Maturation
LC3-1 is activated by ATG7, ATG3 and in conjunction with phospho-ethanolamine (PE) forms LC3-2 that leads to the formation of the mature autophagosome.
Fusion
The mature autophagosome fuses with the lysosome via SNARE proteins and Rab7 to form the autolysosome. The autophagosome releases its contents into the lysosome followed by degradation of the substrates by cathepsins. The macromolecular components are recycled to maintain homeostasis.
How is macroautophagy regulated?
Various signal transduction mechanisms are implicated in the regulation of macroautophagy, in response to various extra- and intracellular stimuli. The three main kinases that regulate autophagy are protein kinase A (PKA), 5’-AMP-activated protein kinase (AMPK) and mTOR complex 1 (mTORC1).
Amino acid signaling and mTORC1
mTORC1 is sensitive to both growth factors and nutrients, and the presence of amino acids is vital for the activation of mTORC1 kinase. Ras-related small GTPases (Rag proteins) activate mTORC1 in response to amino acids. Rag translocates mTORC1 to a specific subcellular compartment that contains the mTORC1 activator Rheb (Ras homolog enriched in brain).
In the presence of amino acids, mTORC1 represses autophagy by inhibiting ULK1 kinase. It does this by directly phosphorylating ATG13 and ULK1 in the ULK1 kinase complex (ULK1-ATG13-FIP200). Under starvation conditions, mTORC1 dissociates from the ULK1 complex, resulting in activation of ULK1. ULK1 auto-phosphorylates and also phosphorylates its binding partners ATG13 and FIP200 to initiate autophagy.
mTORC1 also represses autophagy by directly phosphorylating and inhibiting the ATG14-containing VPS34 complexes in nutrient-rich conditions.
Transcription factor EB controls lysosomal biogenesis and function. Under nutrient-rich conditions mTORC1 and TFEB colocalize to the lysosomal membrane where mTORC1 phosphorylates TFEB, sequestering it to the cytoplasm.
Upon withdrawal of amino acids, mTORC1 is inactivated, and unphosphorylated TFEB translocates to the nucleus where it activates a transcription program that stimulates autophagy.
Energy sensing and AMPK signaling
During an energy crisis, a decreased ATP/AMP ratio is sensed by AMPK and activated through LKB1 kinase. Active AMPK phosphorylates and activates the tuberous sclerosis complex (TSC1/2), which inhibits mTORC1. This stimulates autophagy, which results in increased ATP production via the recycling of nutrients.
ER stress results in an increase in intracellular calcium, which stimulates the calcium-activated calmodulin-dependent kinase kinase b (CAMKKb) to activate AMPK and induce autophagy. In the presence of glucose, PKA is activated by binding with cAMP. PKA inhibits autophagy by indirect activation of mTORC1 through inhibition of AMPK.
Oxygen is an essential nutrient that is required for critical metabolic processes in the cell. Oxygen in conjunction with the electron transport chain in the mitochondria is necessary for generating ATP via oxidative phosphorylation. Hypoxia reduces the ATP levels, activating AMPK and inhibiting mTOR.
mTOR-independent inositol signaling pathway
Autophagy can be induced via an mTOR-independent pathway by lowering the myo-inositol 1,4,5-triphosphate (IP3) levels. This can be accomplished pharmacologically with drugs that disrupt the metabolism of inositol by inhibiting inositol monophosphatase (IMP). Genetic and pharmacological inhibition of IP3 receptor (IP3R) also stimulates autophagy by disrupting the complex formed between IP3R and Beclin 1.
Further Reading